Baby admissions to hospital with common winter virus drop by 80% in trial
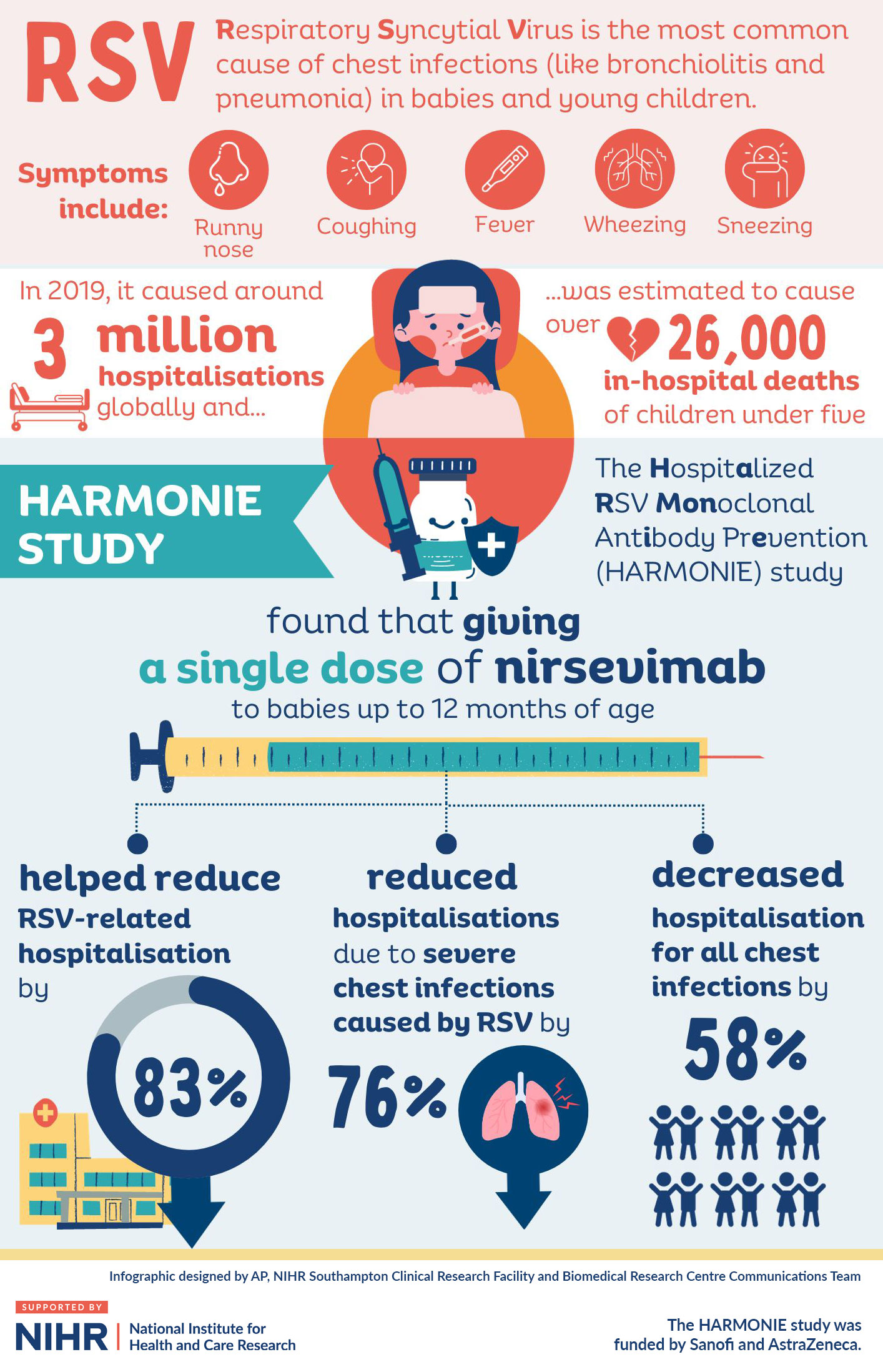
A new preventive treatment to protect babies against a common virus reduced numbers needing hospital treatment by over 80% in an international trial.
The antibody jab offers immediate protection against Respiratory Syncytial Virus (RSV).
RSV is a leading cause of infant hospitalisation. It causes between 20 and 30 infant deaths per year in the UK.
Results from the HARMONIE study, co-led by experts at University Hospital Southampton (UHS), University of Southampton, St George’s University Hospital, and in Primary Care, suggest the antibody jab could help ease winter pressures on the NHS.
The study is a collaboration between Sanofi and the National Institute for Health and Care Research (NIHR).
The new treatment is approved in the UK and is part of considerations for a national RSV immunisation programme. Data from the trial has already been used to roll out the jab in the USA and Spain this winter.
Findings have been published today in the New England Journal of Medicine.
What is RSV?
RSV often causes only mild illnesses, like a cold. However, for some babies, it leads to more severe lung problems such as bronchiolitis and pneumonia.
Most children will have caught it by the time they are two years old.
It is included by some in a so-called ‘tripledemic’ alongside COVID-19 and flu.
The UK’s RSV season typically starts in October, peaks in December and declines by March.
The virus is responsible for around 33,000 NHS hospitalisations annually in children under five years old.
Professor Saul Faust was a co-study leader at the University of Southampton. He is a Consultant Paediatrician at UHS, Director of the NIHR Southampton Clinical Research Facility (CRF) and NIHR Clinical Research Network (CRN) Wessex.
These latest results show that this long-acting antibody is safe and could protect thousands of babies from hospitalisation when used in conditions similar to routine clinical practice. It is really important information for the UK to help decide on options for the future national RSV immunisation programme.
Dr Simon Drysdale, co-study leader and Consultant Paediatrician at St George’s University Hospitals NHS Foundation Trust, London, added:
“RSV is a very contagious infection and every year our wards are full of babies with breathing and feeding problems. The thousands of winter hospital admissions are highly distressing for families and cause a huge winter burden on the NHS. This ground-breaking study shows the potential NHS impact and safety of a monoclonal antibody injection.”
Dr Simon Royal, co-study leader, is a General Practitioner, NIHR National Specialty Lead for Primary Care and Honorary Assistant Professor at the University of Nottingham Medical School. He said:
“This study has shown how primary care clinicians, hospital specialists and the whole UK NIHR system can work together in a new partnership with industry to deliver rapid data to support a critical NHS need.”
European study
The research included 8,058 babies up to the age of 12 months old who were in, or were approaching, their first RSV season. Families took part in the UK, France and Germany.
The phase 3b trial compared nirsevimab, a monoclonal antibody injection, with standard care.
The randomised trial found:
- Hospitalisations for RSV-associated Lower Respiratory Tract Infections occurred in 0.3% (11) of the nirsevimab group. They were seen in 1.5% (60) of those receiving standard care. This equates to an efficacy of 83.2%.
- Very severe RSV-associated Lower Respiratory Tract Infections occurred in 0.1% (5) of the nirsevimab group. They were seen in 0.5% (19) of those receiving standard care. This equates to an efficacy of 75.7%.
- The frequency of adverse events was similar between the two groups, with 36.8% (1,479) in the nirsevimab group and 33.0% (1,326) with standard care. The vast majority were not severe or medically significant.
Antibody approach
Vaccines prompt the body to create antibodies against a target infection, but this can take weeks to happen. However, this injected antibody treatment works straight away to protect a baby against RSV.
Nirsevimab has been shown in previous trials to protect across a whole RSV season from a single injection.
The jab was approved for use in the UK by the Medicines and Healthcare products Regulatory Agency (MHRA) in November 2022.
This summer, the Joint Committee on Vaccination and Immunisation (JCVI) advised that a cost-effective RSV immunisation programme should be developed for both infants and older adults. Nirsevimab is one of the options being considered for RSV prevention next winter.
Globally, RSV is estimated to affect 64 million people and cause 160,000 deaths every year.
This July, the US Food and Drug Administration (FDA) approved nirsevimab for the prevention of RSV-related Lower Respiratory Tract Infections in a baby’s first RSV season, or for those under two years old who remain vulnerable to severe RSV disease.
In Spain, the Andalucía, Galicia and Murcia regions are offering nirsevimab to all babies born during this RSV season and all those who were under six months of age at the start of the season. By March 2024, it is estimated that around 335,000 Spanish babies will be protected.
Study design
The trial had co-leaders from both Hospital and General Practice. This included Prof Faust and Dr Katrina Cathie from UHS and the University of Southampton, Dr Simon Drysdale from St George’s University Hospitals NHS Foundation Trust and St George’s, University of London and Dr Simon Royal, a GP at the University of Nottingham Health Service.
All were integral to a trial leadership group in a streamlined working relationship between the company, NIHR CRN, NIHR Southampton CRF, NIHR Southampton Biomedical Research Centre and study sites. This enabled a rapid study delivery last winter.
The HARMONIE study is funded by Sanofi and AstraZeneca.
