Celebrating NHS 75
5 July 2023 marked 75 years of the National Health Service. To celebrate this milestone, and the way that what we do has evolved and adapted over this time, we took a look back at some of the firsts that have taken place at our hospital. Read about them below.

In 1971, 40 young men and women arrived at Southampton’s new medical school to begin a brand-new degree course. Their arrival was the culmination of several years of planning, preparation and hard work by a team of pioneering academics and clinicians whose innovations would eventually change the landscape of UK medical education.
Find out more in the Southampton medical school, the first 50 years document (produced by the University of Southampton).
In 1986, Professor David Barker found the link between birth weight and lifetime risk for chronic diseases. The discovery is often called the 'Barker hypothesis'.
Following this work, researchers at UHS and the University of Southampton found that chronic diseases in adults may be prevented by early interventions in nutrition, diet and lifestyle of pregnant mothers, infants and children.

In 1993, Professor Sir Stephen Holgate and Professor Ratko Djukanovic, amongst many pioneering respiratory researchers at Southampton, were the first to use a fibreoptic bronchoscopy in asthmatic patients to prove that both inflammation and remodelling of the airways were fundamental to the disease.
Mr Neil Pearce, consultant surgeon, pioneered keyhole surgery for liver cancer in the UK. As a consultant surgeon specialising in pancreatic, liver and neuroendocrine tumours (NETs), he established a world-leading centre in Southampton which he led from 2005 to 2013.
In 2006, a study led by UHS and University of Southampton researchers from the MRC Lifecourse Epidemiology Unit, including Professor Nicholas Harvey and Professor Cyrus Cooper, showed the lower a mother's vitamin D levels during pregnancy, the lower the child’s bone mass tended to be.
As a result pregnant women are now routinely advised to take vitamin D supplements.
More information
Vitamin D regulates the amount of calcium and phosphate in the body, which are needed to keep your bones, teeth and muscles healthy. Government advice is that everyone should consider taking a daily vitamin D supplement during the autumn and winter. However, vitamin D insufficiency is common. In 2006 we invited thousands of pregnant women and their children to take part in a nutritional research study. In this trial, women were randomly allocated to either take an extra 1,000 international units (IU) per day of vitamin D during their pregnancy or a placebo. The results, which were first published in 2006 in The Lancet, showed the poorer a mother's vitamin D levels during pregnancy, the lower the child’s bone mass tended to be. Strong bones in childhood reduces the risk of osteoporosis and fractures in later life. As a result of our findings, pregnant women are now routinely advised to take vitamin D supplements to help increase babies’ bone strength. The research continues to this day, with children from the cohort aged 11-14 being invited to a new research scanning suite at Southampton General Hospital.

In February 2010, the first series of the pioneering One Born Every Minute TV series, was filmed over a period of one month at the Princess Anne Hospital. It was the first healthcare documentary to be made using fixed cameras - 40 in total - and was named best factual series at the British Academy of Film and Television Arts (BAFTA) awards.

In 2011 consultant anaesthetist Dr Ollie Ross, together with anaesthetic colleagues at UHS and videographer Adie Falcinelli, began compiling an adult and paediatric clinical anaesthetic video library.
The library was originally created to support outreach education for nurse anaesthetists working across Nepal but their use is now even more widespread as today the videos are used to support anaesthesia providers globally. Global views now top more than 2 million annually.

Together IT experts and clinicians at UHS, along with Get Real Health, developed and launched the My Medical Record (MyMR) platform which went live in 2012. The tool allows patients to access parts of their record using their devices, including appointments, test results and consultant advice. MyMR is key to patients being in control of their healthcare and in helping the Trust meet our target of an 80% reduction in carbon emissions by 2032. The platform has been adopted by many other organisations both in the UK and beyond.

In 2014, Professor Hasan Arshad, a UHS consultant and chair of allergy and clinical immunology, led the team to become recognised as the world's first ever centre of excellence, which was testament to the hard work of the researchers and clinicians dedicated to improving patient care and research.
Read the NIHR Southampton Biomedical Research Centre press release here.

In the summer of 2017, Dr Alex King, Mr Tim Dudderidge, Dr David Breen and support teams used MRI guided prostate cancer cryotherapy. The technique uses frozen needles guided by magnetic resonance imaging (MRI), offering cancer treatment to some patients previously unsuitable for conventional curative options. We remain the only UK facility to use this effective technique.
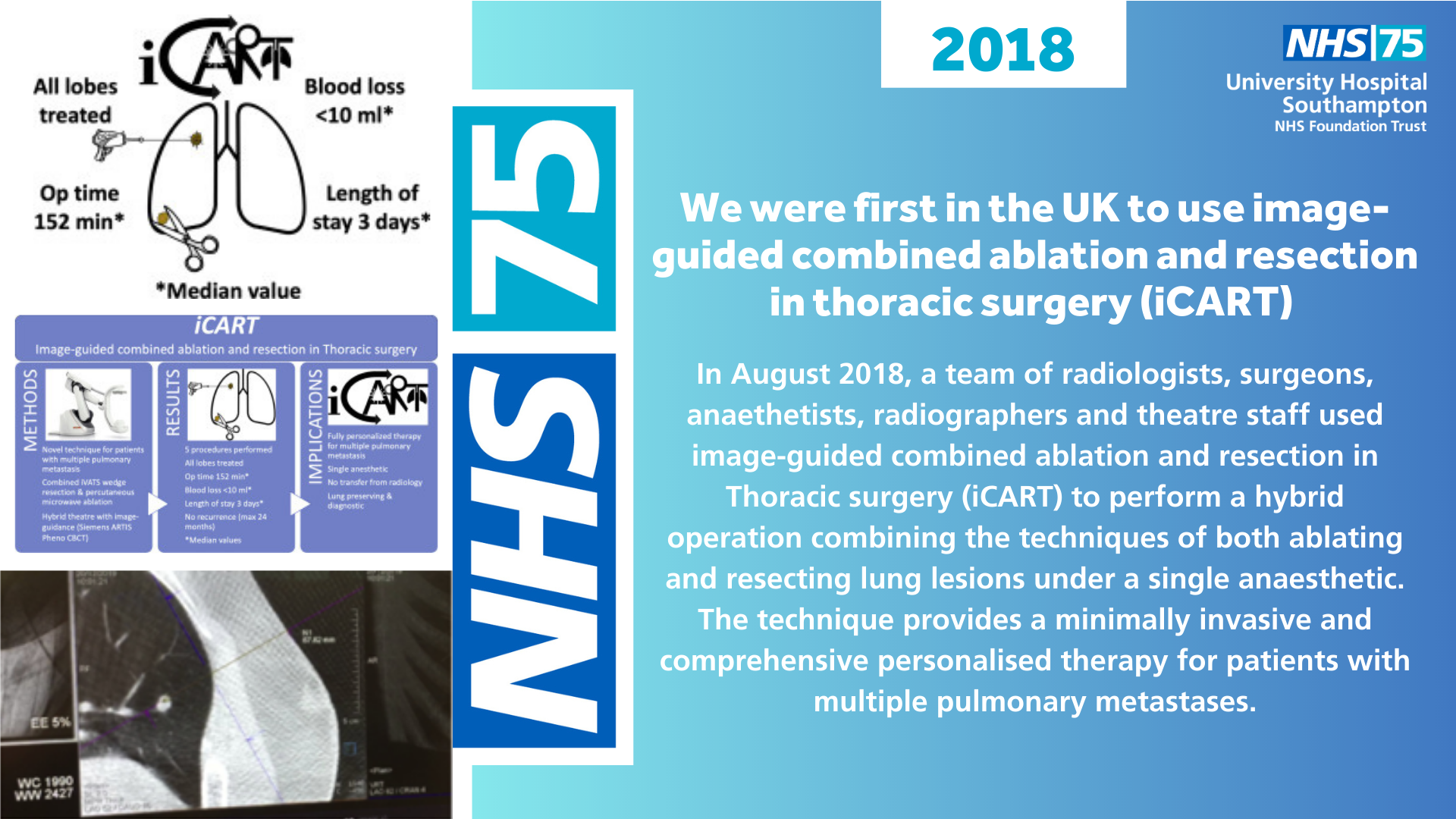
In August 2018, a team of radiologists, surgeons, anaesthetists, radiographers and theatre staff used image-guided combined ablation and resection in thoracic surgery (iCART) to perform a hybrid operation combining the techniques of both ablating and resecting lung lesions under a single anaesthetic providing a minimally invasive and comprehensive personalised therapy for patients with multiple pulmonary metastases.
More information
Image-guided combined ablation and resection in thoracic surgery (iCART) is a hybrid operation which combines the techniques of both ablating and resecting lung lesions under a single anaesthetic. Ablation involves inserting a needle into the lung and delivering microwaves or radiowaves to ‘cook’ the cancer. Resection involves passing a wire into the tumour and then using key hole surgery to remove the lesion as a wedge resection with a stapling device. The technique was developed in order to reduce the number of operations that a patient with multiple lung nodules would traditionally have to undergo so this hybrid approach provides a minimally invasive and comprehensive personalised therapy for patients, providing histology-based diagnosis whilst minimizing lung tissue loss and eliminating the need for transfer from radiology to operating theatre.

In 2018, working in partnership with University of Southampton, we opened the UK's first centre dedicated to accelerating cancer immunology research.
Today, the Centre for Cancer Immunology is expanding clinical trials, exploring new areas and developing lifesaving drugs.
More information
In 2015 the University of Southampton launched a £25 million campaign to build the UK's first centre dedicated to cancer immunology research. The target was reached six months ahead of schedule, with the centre opening in spring 2018 at Southampton General Hospital. Immunotherapy is a revolutionary approach to treatment that uses the body’s own immune system to fight cancer. This cutting-edge research hub enables interdisciplinary teams to expand clinical trials, explore new areas and develop lifesaving drugs. For more than 40 years, Southampton researchers have been at the very forefront of cancer immunology research and have an international reputation for bench to bedside results. Today, scientists from the Centre for Cancer Immunology are turning basic scientific discoveries into meaningful treatments that will improve patients’ lives. Ongoing research includes a world-first clinical trial to test a new treatment for neuroblastoma, one of the most common childhood cancers.

A pioneering study, led by Gorav Datta, a consultant orthopaedic surgeon at University Hospital Southampton developed a new customised treatment for knee arthritis patients which saw the use of hyaluronic acid combined with platelet-rich plasma taken from each individual. The treatment was designed to achieve longer-lasting pain relief with better knee joint function without the need for steroid injections.
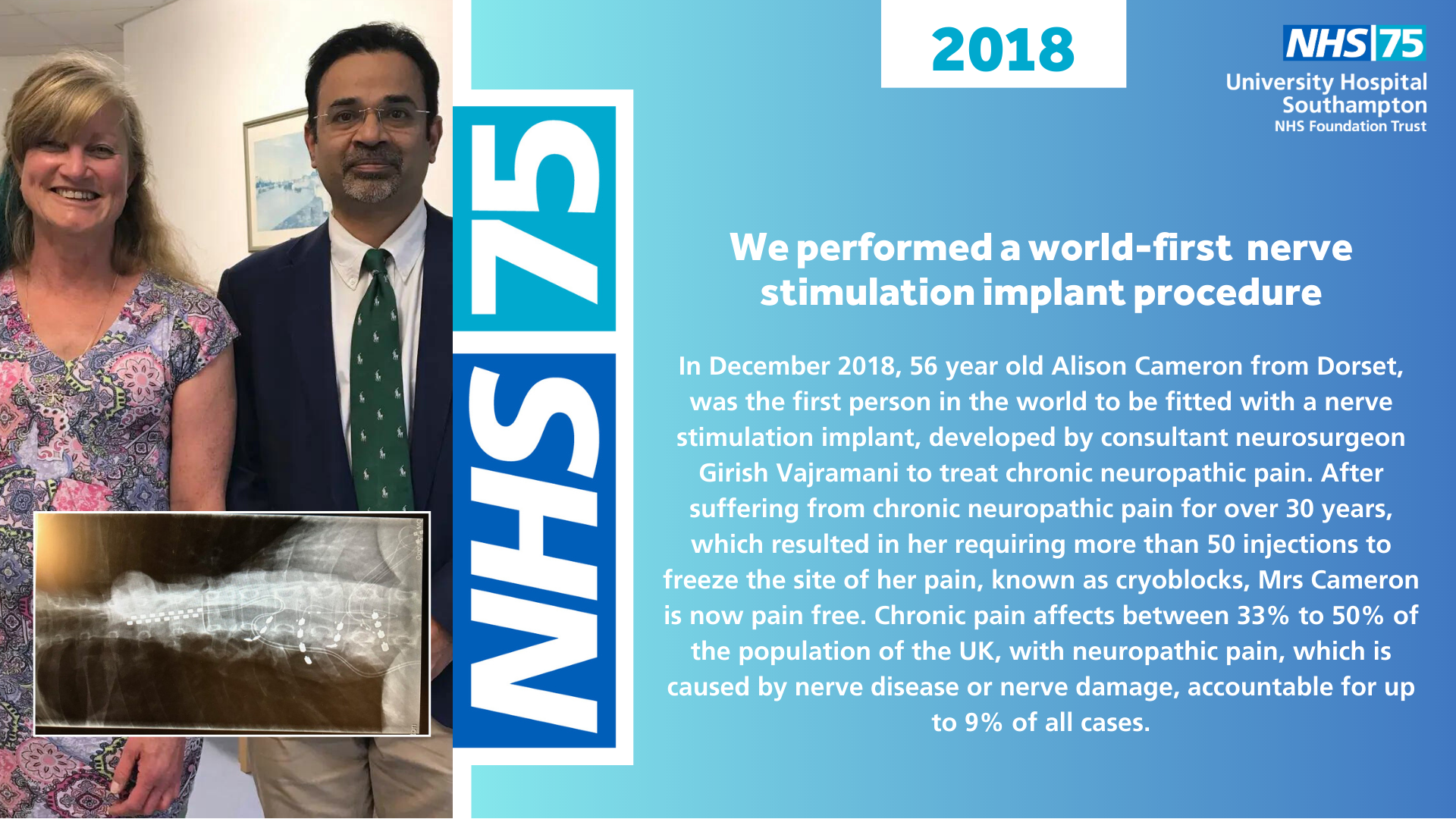
In December 2018, 56 year old Alison Cameron from Dorset, was the first person in the world to be fitted with a nerve stimulation implant, developed by consultant neurosurgeon Girish Vajramani to treat chronic neuropathic pain. After suffering from chronic neuropathic pain for over 30 years, which resulted in her requiring more than 50 injections to freeze the site of her pain, known as cryoblocks, Mrs Cameron is now pain free. Chronic pain affects between 33% to 50% of the population of the UK, with neuropathic pain, which is caused by nerve disease or nerve damage, accountable for up to 9% of all cases.

In February 2019, Southampton Saints fans attending a match at St Mary's Stadium were invited to attend pre-match screening for type 2 diabetes. Screening was carried out by clinicians led by Dr Mayank Patel, a consultant in diabetes at UHS, and nurses from Solent NHS Trust.
The scheme was funded by Southampton Hospitals Charity and supported by Saints Foundation and the Diabetes Research and Wellness Foundation and was the brainchild of Dr Mike Sadler. 7% of the 103 fans who verbally consented to a point-of-care HbA1c test had an abnormal result.

In 2019, consultant ophthalmologist Professor Parwez Hossain, became the first eye expert in the UK to use precision laser to split corneal tissue, when he operated on 36 year old Daniel Hackling from Totton Southampton, who became the first patient to undergo a corneal transplant using the laser.
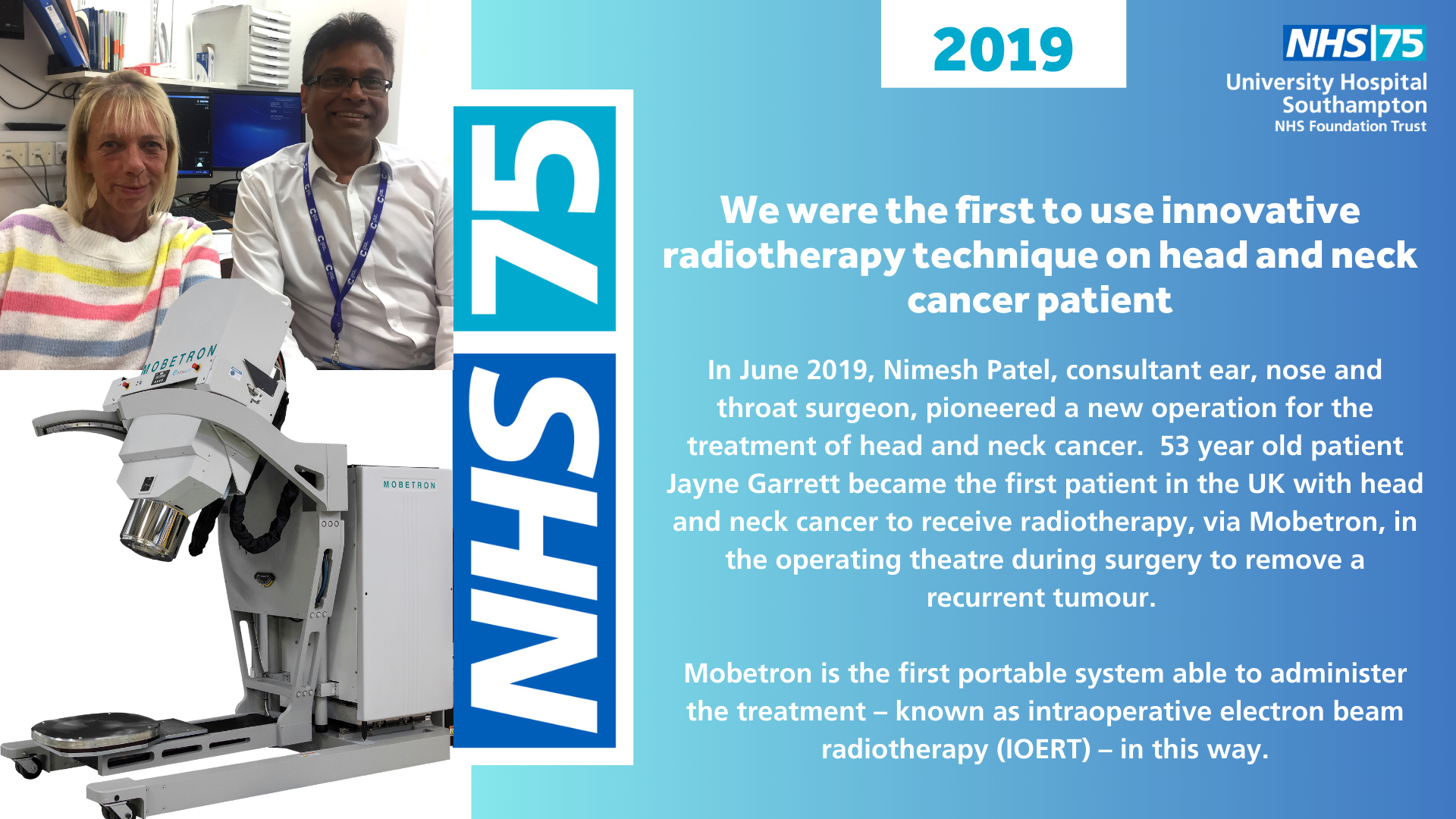
In June 2019, Nimesh Patel, consultant ear, nose and throat surgeon, pioneered a new operation for the treatment of head and neck cancer. 53 year old patient Jayne Garrett became the first patient in the UK with head and neck cancer to receive radiotherapy, via Mobetron, in the operating theatre during surgery to remove a recurrent tumour.
Mobetron is the first portable system able to administer the treatment – known as intraoperative electron beam radiotherapy (IOERT) – in this way.
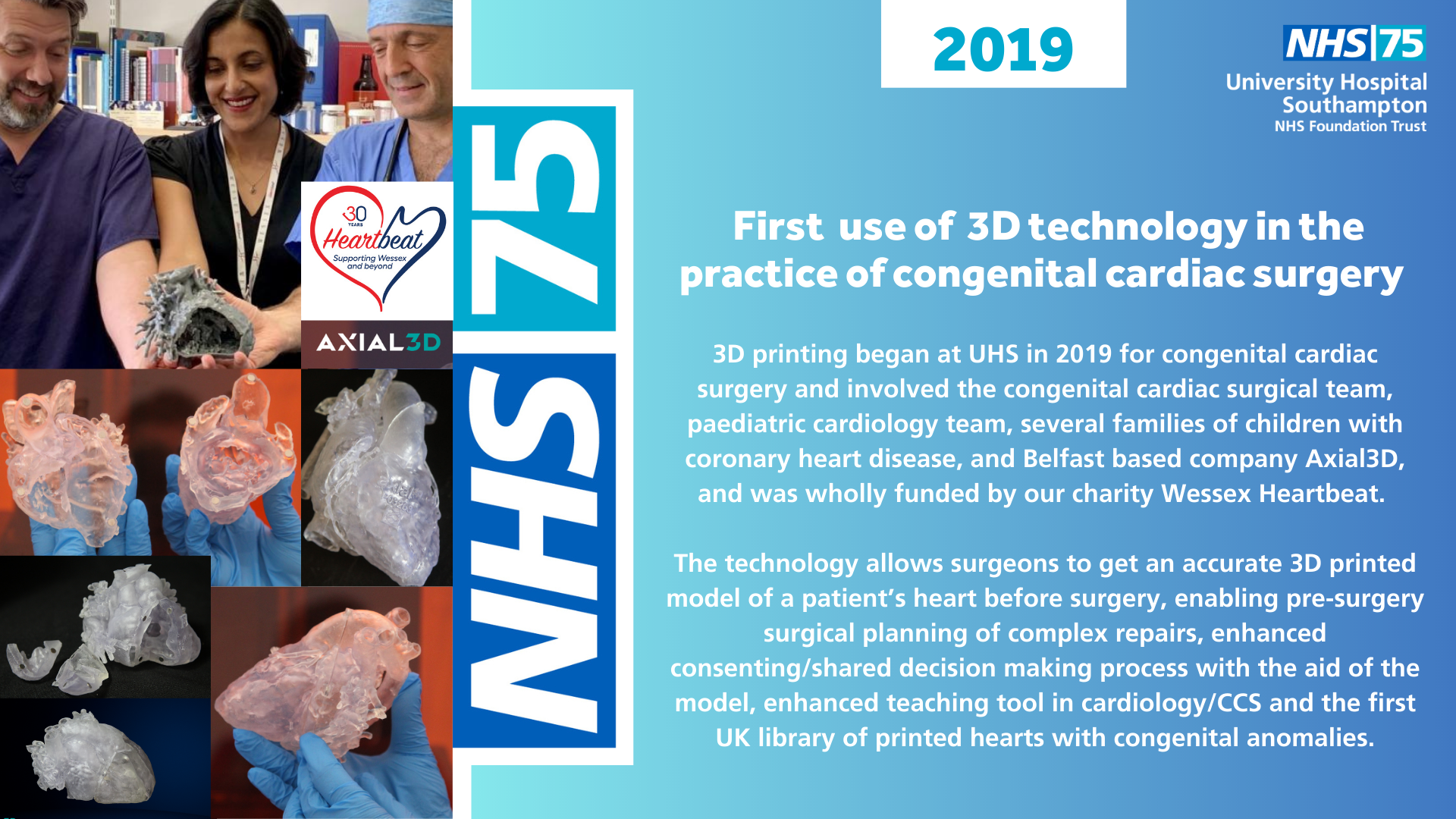
3D printing began at UHS in 2019 for congenital cardiac surgery and involved the congenital cardiac surgical team, paediatric cardiology team, several families of children with coronary heart disease, and Belfast based company Axial3D, and was wholly funded by our charity Wessex Heartbeat.
The technology allows surgeons to get an accurate 3D printed model of a patient’s heart before surgery, enabling pre-surgery surgical planning of complex repairs, enhanced consenting/shared decision making process with the aid of the model, enhanced teaching tool in cardiology/CCS and the first UK library of printed hearts with congenital anomalies.

Adult consultant urological surgeon Bhaskar Somani, who is skilled in the use of an advanced minimally-invasive procedure ureteroscopy, worked alongside paediatric urological surgeon Stephen Griffin to create the 'twin surgeon' model to remove kidney stones in children.
Ureteroscopy involves inserting a thin tube used for viewing into the kidney via the bladder to visualise the stones before removing them using a small forceps-like tool or a laser beam to break them up. The innovative ‘twin surgeon’ model has led to complete removal of stones in 99% of cases.

Launched during the first wave of the Covid pandemic, the Patient Support Hub was initially created to support a number of patients who were shielding due to medical conditions. Since then the Hub, thought to be the first of its kind in the country, has grown into a wider support network which brings together volunteers and community providers to focus on patients’ wider needs.
Funded by the Southampton Hospitals Charity, the National Lottery and NHS Charities Together, the project now offers services including delivery of food parcels and shopping, collection of prescriptions, befriending and signposting to other services in the community.

In collaboration with the University of Southampton and industry partners we developed a prototype reusable, battery-powered respirator (known as the PeRSo hood) as an alternative PPE to standard disposable face masks.
The PeRSo hood overcame the reliance on disposable face masks, of which there was a global shortage at the time, and were far more comfortable to wear. Additionally they meant that they could be worn for longer periods of time. The prototype was driven into production in under a month. The PeRSo hood is now certified for all use as PPE by the British Standard Institute.

The Banksy 'Game Changer' artwork was installed in University Hospital Southampton (UHS) in May 2020 as a thank-you to staff during the first wave of the Covid-19 pandemic. On 23 March 2021, on the day of national reflection in the UK, Banksy auctioned the original canvas, donating the funds raised to Southampton Hospitals Charity to support a range of staff wellbeing projects.
A reproduction of the work remains in the C level East Wing lift lobby at Southampton General Hospital.

Lyndsey Uglow and Leo were announced as the winners of the Kennel Club Friends for Life competition at Crufts 2020.
Leo has been visiting adults and children on the wards since 2012, initially starting as a Pets as Therapy (PAT) representative through the voluntary services team at University Hospital Southampton NHS Foundation Trust.
Leo is now part of the animal assisted intervention (AAI) team led by Lyndsey at Southampton Children’s Hospital who visit children to help create positive memories of the healthcare environment.

Ortho-plastic fix and flap, which is a surgical limb reconstruction with circular frame, bone lengthening and microscopic free tissue transfer, was jointly performed for the first time at UHS in March 2021 on Mr Philip Devereux, by consultant orthopaedic surgeon Ms Jo Round and consultant plastic surgeons Mr Gavin McCoubrey, Mr Paul Stephens, Ms Rebecca Exton, and Ms Jessica Steele supported by the ortho-plastics CNS and ward/theatre teams.
This meant that all definitive treatment was performed in our hospital for the first time, reducing the amount of operations a patient would have to undergo, reducing their length of stay in hospital and reducing delays and freeing up valuable theatre time.
More information
In the past patients with open fractures requiring soft tissue microscopic surgery would be required to transfer to Salisbury District Hospital for plastic surgery reconstruction. However, when the COVID-19 infection struck, the infection prevention protocols meant that we were no longer able to transfer patients between trusts. So we had to think differently. We expanded our ortho-plastics trauma service so that procedures requiring both orthopaedics and plastic surgery could be performed in a single hospital. This prevented delays associated with transferring to other hospitals and crucially, because ortho and plastics were together in the theatre at the same time, they we able to discuss and make decisions at the time, thereby reducing the total amount of operations a patient required and reducing their length of stay in hospital.
In 2021, results of a trial led by Southampton's Prof Saul Faust, showed six COVID-19 vaccines were safe to use as a third dose booster jab.
This information was key to shaping the UK booster programme and gave vital evidence for global vaccination efforts.

In 2022, Professor Paul Roberts, consultant cardiologist at UHS, led the medical team to implant the first UK leadless pacemaker defibrillator system into 56 year old patient David Mills, a retired policeman from Southampton.

In 2022 we were awarded £29.4m from the Public Sector Decarbonisation Scheme to fund a major new energy-efficient heating system fit for the future. The state-of-the-art new system will help UHS take great strides towards its pledge to become Net Carbon Zero by 2045, as set out in the Trust’s Green Plan launched in April 2022 – reducing CO2 emissions by an estimated 4881 tonnes per year.

We partnered with Jacksplace, a hospice for young adults, to create the UK’s first one-stop clinic in a joint venture with the voluntary sector for patients with Duchenne muscular dystrophy (DMD).
The specialist clinic, based at Naomi House & Jacksplace in Winchester, runs every other month and combines appointments with different health professionals all in one day – meaning patients don’t need to come into hospital as often to have their condition monitored.

In 2022, we launched a new self-referral service for men who have symptoms of prostate cancer or are at higher risk of developing it, following a dramatic drop in referrals which led to a decrease of 23% in men starting treatment across the region at the height of the Covid-19 pandemic.
The service focuses on improving access to specialists, raising awareness of early symptoms and information about testing. If considered high risk after completing an initial assessment questionnaire, men will be offered a range of investigations without the need for a GP referral.

In March 2023 Dr Andrew Flett, Dr Peter Cowburn, CV+T research team (Alix Baird) and FIRE1 team implanted the first FIRE1 IVC heart failure monitoring system in the UK.
The unique technology is a sensor about the size of a pen lid which is designed to monitor the amount of fluid in the body – elevated levels can give an indication of worsening heart failure. Patients can be monitored remotely for fluid status with the aim of preventing fluid build up and acute admissions to hospital.

On 15 May 2023, Mr Lukacs Veres Consultant Thoracic Surgeon, led the team to perform the world's first simultaneous multiplatform robotic lung resections -using both the Da Vinci and CMR Versius robot systems.
We have now performed over 300 major lung resections robotically and data suggests that these patients have less pain, less blood loss, shorter hospital stay and quicker recovery.

In May 2023, Sam Matthews, prostate diagnosis nurse practitioner, became the first non-consultant worldwide to gain competence in Barrigel rectal spacer insertions. With oversight from Mr Chedgy (consultant urologist), Sam led the redesign of the suspected prostate cancer service (referral to diagnosis) transitioning it from consultant led to nurse led. Her skills in transperineal prostate biopsies developed during this time, paving the way to enable her to offer rectal spacer insertion. The procedure helps reduce urinary and bowel toxicity and improves the patient's quality of life.
In 2023, we became the first in the world to pilot a new at-home diabetes test for pregnant women.
The finger prick blood test works in the same way as the traditional in-hospital oral glucose tolerance test (OGTT) but can be carried out by the patient at home, avoiding the need for a clinic appointment.

The hybrid operating theatre in SGH, (surgical theatre with additional hardware for angiography), involves a team of neurosurgeons, interventional neuroradiologist, anaesthetic and hybrid operating theatre team and our radiographers.
This combined approach means open brain surgery and x-ray intervention for this complex condition can be done in the same setting, improving treatment success rate and reducing recurrence as well as avoiding unnecessary extra anaesthetic procedure later on.
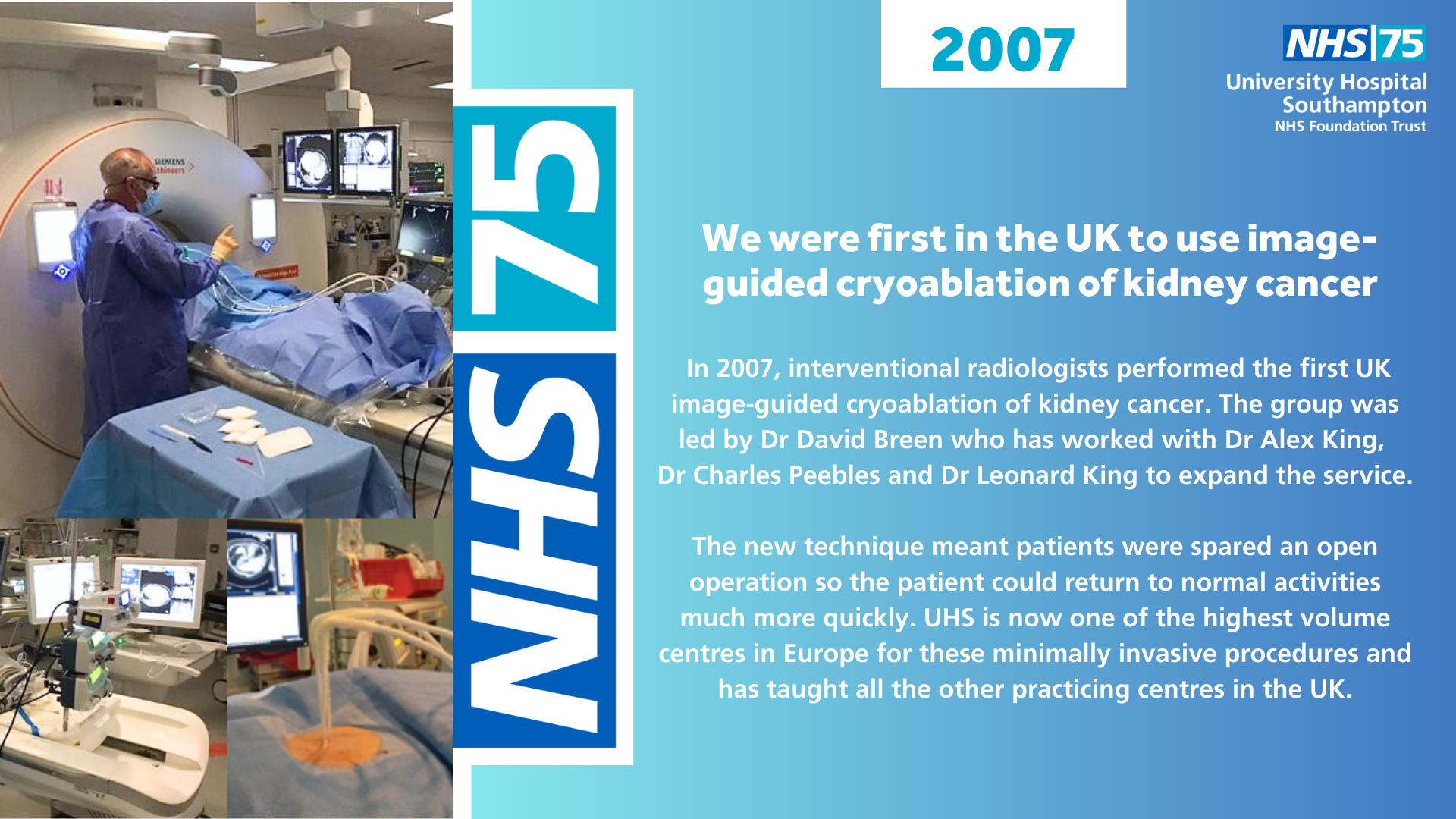
In 2007, interventional radiologists performed the first UK image-guided cryoablation of kidney cancer. The group was led by Dr David Breen who has worked with Dr Alex King, Dr Charles Peebles and Dr Leonard King to expand the service.
The new technique meant patients were spared an open operation so the patient could return to normal activities much more quickly. UHS is now one of the highest volume centres in Europe for these minimally invasive procedures and has taught all the other practicing centres in the UK.
Watch a YouTube video on image-guided cryoablation in kidney cancer.
In 2008 our cardiothoracic MR team introduced our radiographer led cardiac MRI stress service. This new service saw radiographers trained to supervise the administration of Adenosine. The new service meant patients could have the examination on any weekday, increased efficiency and capacity and, most importantly, reduced patient waiting times.
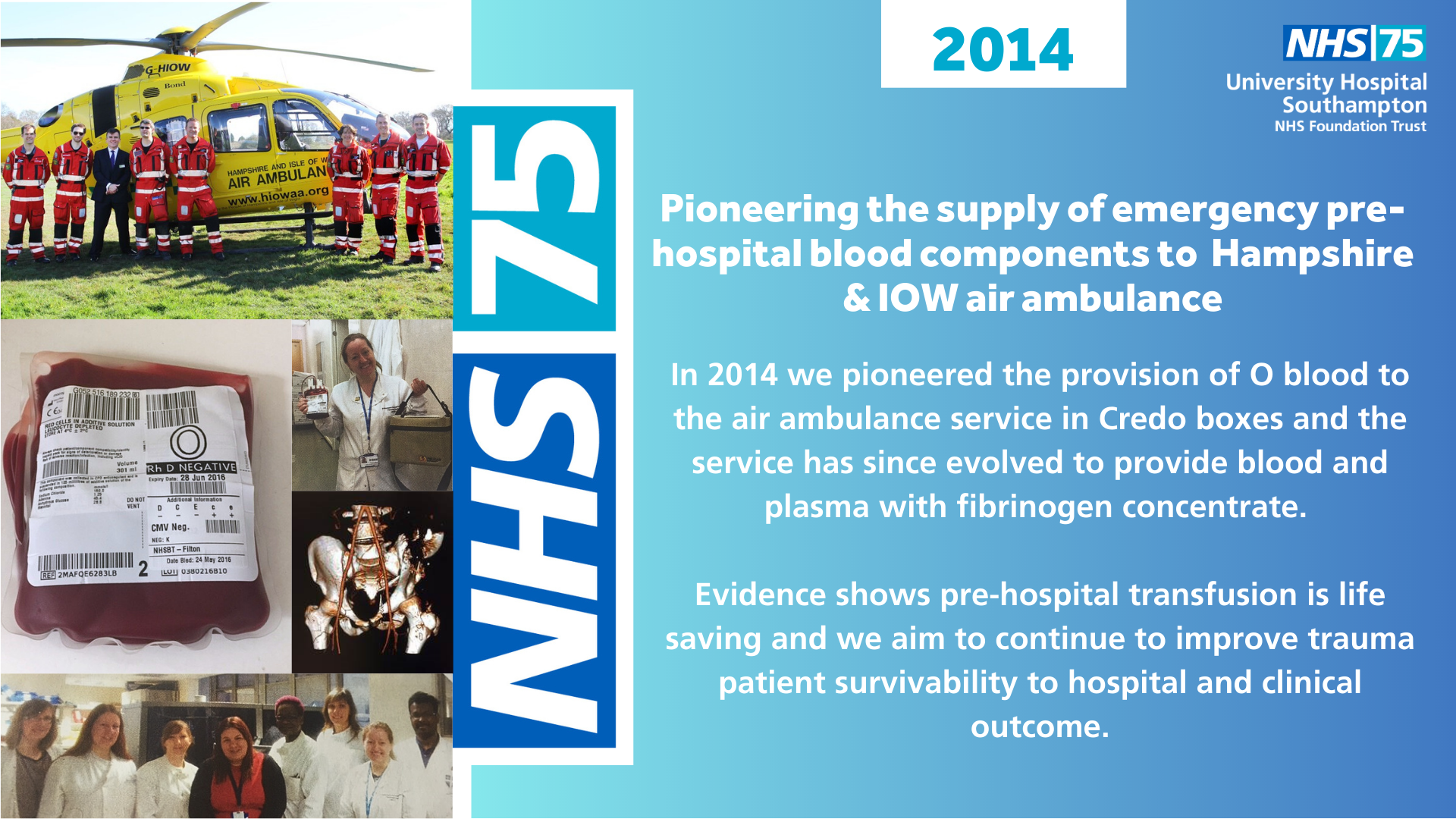
In 2014 we pioneered the provision of O blood to the air ambulance service in Credo boxes and the service has since evolved to provide blood and plasma with fibrinogen concentrate.
Evidence shows pre-hospital transfusion is life saving and we aim to continue to improve trauma patient survivability to hospital and clinical outcome.
More information
Practical evidence emerged which demonstrated that pre hospital transfusions can be lifesaving, including strong evidence from military operations and so, with the Hampshire and IoW air ambulance, we looked at how we could improve the number of trauma patients surviving long enough to be transferred into our care at the Major Trauma Centre. We began by supplying the air ambulance service with O blood and then, over the years, we have been able to supply more sophisticated blood components (including blood and plasma with fibrinogen concentrate) which enable the air ambulance team to treat the patient more effectively at the scene and during transportation, therefore improving patient survivability to hospital.

In 2016, Dr Andrew Flett, Dr Peter Cowburn, Abbott cardiology and Sian Mackay were the first in the UK to use clinical implants of a pulmonary artery pressure monitoring system to guide heart failure management.